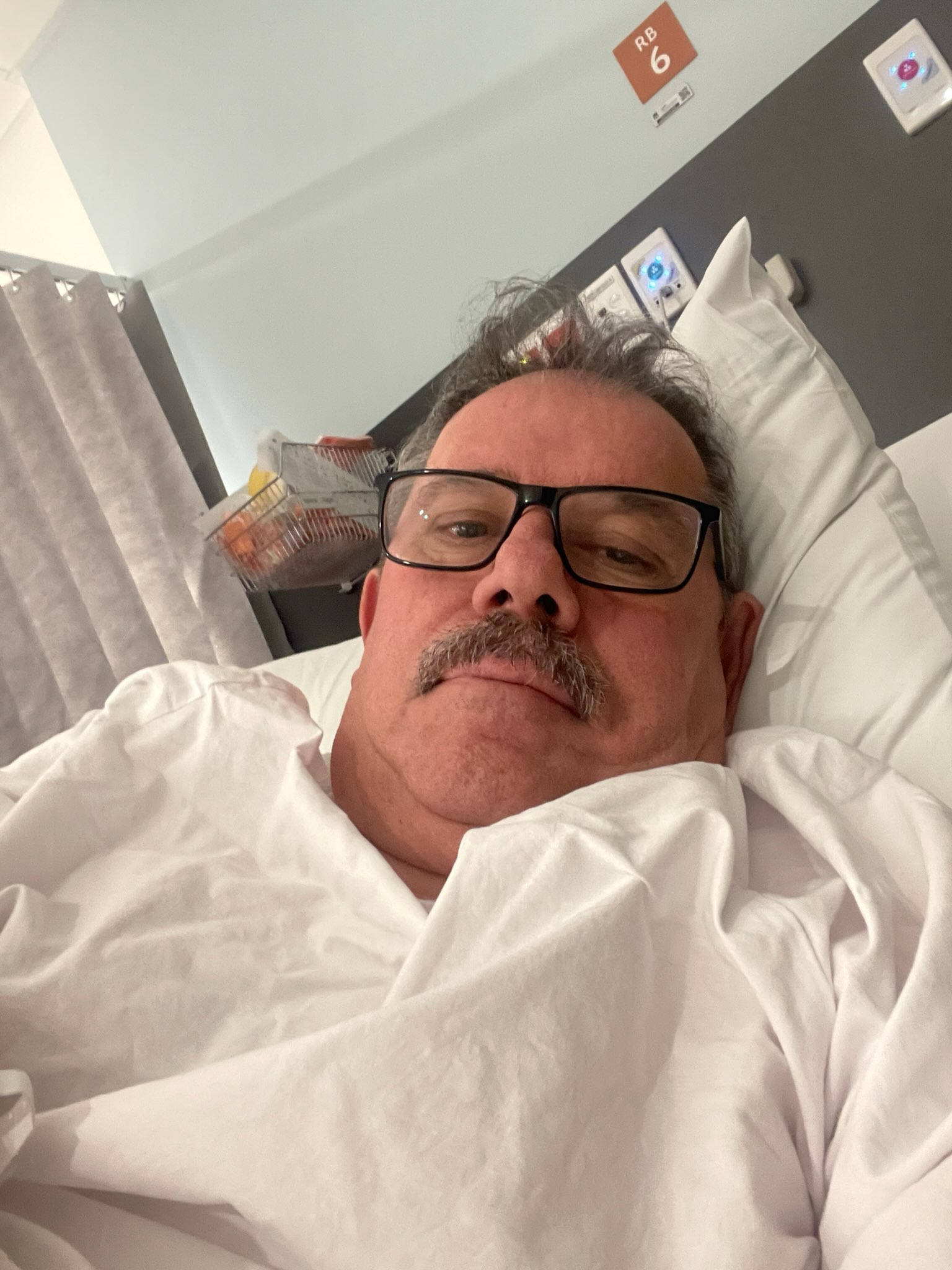
Brad Lancaster warns men to have annual PSA checks after prostate cancer scare
Simon Mumford
19 July 2025, 9:00 PM

Lismore local Brad Lancaster has a warning for the men of the Northern Rivers: get a simple PSA blood test to avoid more major physical and emotional decisions later.
Cancer Australia says that there were an estimated 26,368 new cases of prostate cancer in 2024. It is also estimated that a male has a 1 in 6, or 18%, chance of being diagnosed with prostate cancer by the age of 85.
Brad Lancaster is now one of those statistics.
Brad was doing the right thing, getting regular blood tests to check his PSA (prostate-specific antigen) level, which was always around the 4 mark. In November last year, he received the news that his PSA had doubled to 8 within 12 months.
Brad's doctor requested a second blood test in January 2025, in case there was a false reading due to a urinary tract infection or another variable. That test returned an 8.5 reading.
The next step was a referral to a urologist, which was only a 2-3 week wait. An MRI scan was ordered to check for the presence of cancer cells. Another positive result led to a biopsy.
"They go in and take little samples, about the size of cotton threads. They take core samples. And she ended up doing 36 samples on it. Of those 36 samples, 14 were cancerous."
Brad explained that from those results, you get a Gleeson score between 5 and 10 that indicates how quickly the cancer will grow. 5 is on the lower level, and 10 is on the aggressive side.
"I ended up with a five plus a four, which gives you a nine. The first one is the worst one. So, a five has been the aggressive one, and the next lot was a four, so it was nearly as aggressive."
With a 9 Gleeson score, Brad's medical treatment was fast-tracked with a PSMA PET scan, a new type of scan used to detect and stage prostate cancer, a CAT scan and x-rays to get a complete overview of the cancer in the prostate and to see if it had spread to other parts of his body.
"The next day, I got a phone call from the Lismore Cancer Clinic. I had the option of either radiation or the robotic removal of the prostate."
After a two-hour consultation with a radiologist in Lismore, Brad learned about the effects of radiation on his body.
"The option was to have 20 doses of radiation over a month. So, you do Monday to Friday, and it's only a quick process, about 10 to 15 minutes. You have to be sort of consistent, so your bladder has to be so full and your bowels have to be empty."
Brad has also had two hip replacements, which could have affected his radiation treatment, given the location of the prostate. Deflection of the pinpoint radiation was a concern because it needed to target all parts of the prostate, rather than a specific location.
"Then, on top of that, it would have been six weeks of hormone therapy before the radiation starts, and then 18 months to two years of hormone therapy afterwards," Brad recalled.
"With the hormone therapy, it basically kills the testosterone in your body. The side effects of the ADT or the hormone therapy are that it basically kills your manhood in a way."
Testosterone is primarily produced in the testicles. The prostate gland relies on testosterone for its function and development. Hormone therapy blocks the testosterone levels to slow down or stop the cancer cell growth.
Brad had two choices. Radiation treatment and hormone therapy, or the complete removal of the prostate.
Brad chose the removal of the prostate. This was to be done at the Nepean Hospital in Sydney as part of the public health system.
This is where Brad potentially encountered another complication: he is a little person.
"I'm the first little person in Australia to get the operation done with a robot. They were questioning if they could do it or not. They rang doctors in the UK and America to see if they'd performed the procedure. In the end, I sort of made the decision to just go with the removal of it. And, the doctor said he wanted it all out within 30 days because of the Gleeson score of nine."
Part of the pre-operation procedure is performing pelvic floor exercises to minimise the incontinence post-surgery.
"There is a lot of support. I had Jessica from the public health system at the Base Hospital, she's a prostate support nurse, give me a whole lot of information. She was ringing every two weeks before the surgery to check up on me because it is an emotional roller coaster. In the meantime, I saw David Hughes, he's a private prostate support nurse, who has some valuable YouTube videos that explain a lot. Everyone is different. It could be good for me or bad for me; it all depends on your age and if you're active and fit, which I'm neither.
Brad has had to change his eating habits to lose weight before the surgery due to body fat and to aid his recovery. He is now drinking green tea and eating a healthy, balanced diet.
It has been nine weeks since Brad's prostate removal. His latest blood test revealed a PSA of 0.008, which he said is the lowest that Sullivan Nicolaides can go in their testing.
"So, the way they describe it, I've got no detectable cancer," Brad smiled. "I'm not cancer-free at this stage, but I've got no detectable cancer. Every three months now, I'll do another PSA test to make sure it stays there. And if it goes above, if it does creep up, which it could creep up with some microcells still floating around the system, a PET scan will only pick up a clump of cells when they've actually attached to something. So there could be microscopic cells floating around.
There are two health issues that Bradnow needs to consider: incontinence and erectile dysfunction.
"The incontinence is more with the removal side of it, because when they cut the prostate out, they've got to join your urethra back to the bottom of your bladder, so you lose one of your main muscles that controls your urinary stop, start and all that, your memory one, but there is another muscle below it that you manually have to try and use and train. I'm back to about 98% I'd say now. I'm getting better and better all the time.
"This does affect a lot of relationships where partners break up because the other side effect is the ED, erectile dysfunction. All the nerves are wrapped around the prostate, so a lot of times they can spare the nerves, but it can take up to a year or so for all the actions to come back. And they may be half as good, or for others, they can't save the nerves at all. But there are operations that they can put in a sling, and then there is medication or injections to get you through that drama.
"But the main thing is you're alive, you're on the top side of the grass, instead of on the other side. I took the risk with the operation, and now, hopefully, I'll get 15 years or more, or maybe longer."
Brad has found that support groups have helped him during his prostate cancer journey.
"I'm part of support groups on Facebook. There's a very good Prostate Australia Facebook group. It's a private group, so it's not out there in the public, and guys discuss what goes on. I'm pretty open about what it is, I'd rather talk about it than hide it, but it's not a walk in the park."
Brad wanted to tell his story to warn the men of Lismore and the Northern Rivers that prostate cancer affects more and more males each year, and it is not a pleasant disease.
"Everyone said, Oh, it's an old man's disease. But it's getting younger and younger. There's a lot of guys in their 50s, and even some in the 40s. And there's another group that I joined the other day in South Australia, that had guys who are in their 40s that have got prostate cancer. And that's the thing, because no one sort of caters for them. They're still active and fit and working, and it messes with your life, the emotional rollercoaster, as I said before, you're up and down all the time.
Brad's advice is to get your blood tested once a year.
"It's only a tick on the box when you're getting a blood test. So, if you're going for a yearly checkup, they do a blood test, and men should say, Well, check my PSA too. In one year, I went from a PSA of four to eight, and I had no symptoms. If I didn't check it, or I didn't say, I'll wait two years to get it done, it could have metastasised. It could have been through my body then, and we would be having a different conversation right now."
"But the signs are good, it's been a great outcome, and it's been a great recovery. It's just another hurdle in life. I didn't want this, but you've just got to adapt and go with it."

